By Serena Mahalingam
In 2008 the World Health Organization created the Commission on Social Determinants of Health to awaken society to the influences of social factors on health and health inequities. Though not a new idea, the commission felt it important to bring together policy makers, researchers, and other stakeholders to gather evidence on how to achieve a more just distribution of health worldwide. Since then, recent changes in American legislation, reimbursement structures, and public perception have drawn even more attention to the issue. A PubMed search for articles featuring the term “social determinants of health” finds that though the first article was published in 1961, 79% of the articles have been published between 2008 and now, revealing the recent upsurge of interest in the concept.
For those not in the public health industry, however, there is still a widespread lack of awareness about this term and its implications. For many, social factors are generally seen as far less important to health than they actually are.1 To illustrate how intertwined social factors and health can be and to address the shortage of general knowledge about SDoH, this article presents an example of how one social need – transportation – can influence individual-level health and how it can result in population-level consequences.
What makes a person healthy?
In response to this question, you may think of health behaviors, such as diet, exercise, and smoking, as well as clinical services such as vaccines, medicines, and surgeries. You may even think of environmental conditions such as water sanitation or air pollution. While it is true that all of these factors do play an important role in our health, research demonstrates that no factor impacts our health more profoundly than social and economic factors, often referred to in healthcare as social determinants of health (SDoH).2 As Amber wrote in our last blog, social determinants of health are defined as the conditions in which people grow, learn, work, and live. Some examples of these determinants include availability of affordable housing, gender inequity, educational opportunities, and access to transportation.
An illustration: transportation
For a simplified illustration of the overpowering impact these factors can have on our health, consider the factor of transportation. A person who owns a dependable vehicle likely has the easiest access to healthcare in terms of this factor, though in certain regions of our country the closest healthcare provider may still be hours away.
Next, consider a bus-rider who is lucky to have an affordable route with a stop near their home. In the best-case scenario, this person can get to a healthcare provider by taking one bus, but more than likely, will have to switch buses, which can be both costly and time-consuming. Additionally, pharmacies, grocery stores, and other healthcare specialists take effort and time to reach.
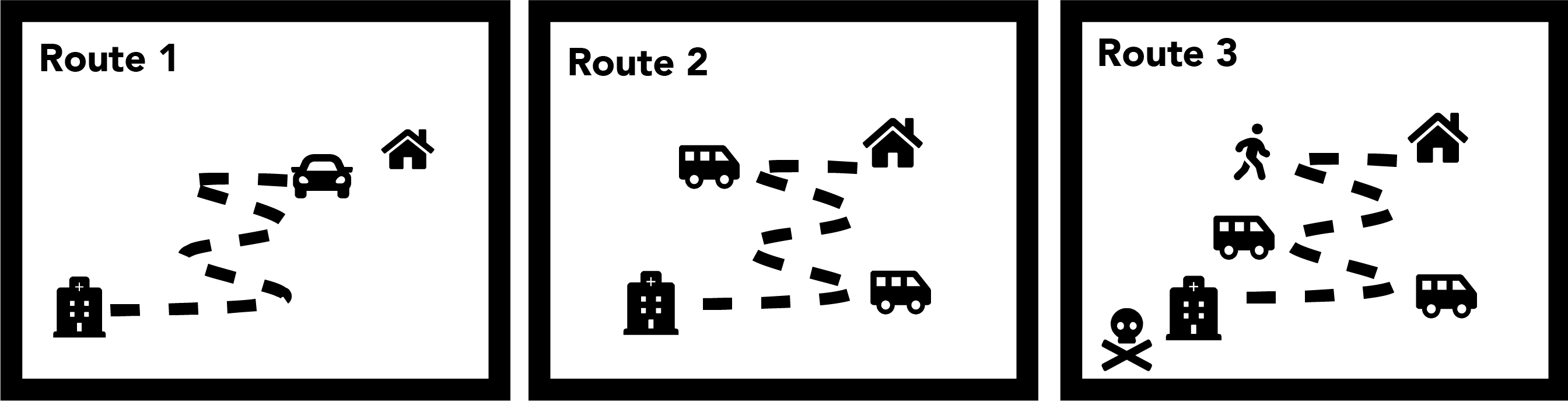
Now, imagine having neither access to a car nor nearby public transportation. Some healthy people may adapt by walking several miles to the nearest plaza or public transit stop. However, consider someone who has asthma, and consequently avoids walking on the dirt roads near his home for fear of triggering an asthma attack. This person will likely not get medical care until an emergency arises and he has no choice but to call an ambulance. The deterioration of his health as well as his exorbitant medical bills resulting from an emergency room visit potentially could have been avoided if his transportation situation had been different. This is how social and economic factors that initially appear to have no connection to our health actually end up holding the largest share in it.
In acknowledgement of this, numerous payers, health care providers and advocacy groups across the country have implemented pilot transportation programs that support patients with transportation barriers. These programs often have the goals of reducing missed appointments and improving patient transportation experiences.
National Impact
Beyond the effect that social determinants have on the individual level, they also have a large influence on healthcare nationally. For example, missed appointments cost our country $150 billion annually and medication non-adherence adds another $290 billion to our healthcare costs each year.3 Looking again at transportation, you can imagine the wonders increased access to transportation could do to proliferate the number of patients who could make it to their appointments and fill their prescriptions.
Addressing SDoH has the ability to not only advance health outcomes on an individual basis, but on the population level as well. In 2018, healthcare spending equated to $3.65 trillion.4 Despite ranking 1st on healthcare spending internationally, we merely rank 27th for level of healthcare.4 Moreover, one U.S. study found that 68% of patients have at least one SDoH challenge.5
These statistics represent stark challenges in the current sphere of health policy. Luckily, the solution to lowering both our healthcare spending and the percentage of patients with SDoH challenges is identical: investing time, money, and resources into addressing the socio-economic needs of patients.
Reference List
- Haslam SA, McMahon C, Cruwys T, Haslam C, Jetten J, Steffens NK. Social cure, what social cure? The propensity to underestimate the importance of social factors for health. Soc Sci Med. 2018; 198: 14-21. doi: 10.1016/j.socscimed.2017.12.020
- Hood CM, Gennuso KP, Swain GR, Catlin BB. County Health Rankings: Relationships Between Determinant Factors and Health Outcomes. Am J Prev Med. 2015; 50(2): 129-135. doi: 10.1016/j.amepre.2015.08.024
- Sviokla J, Schroeder B, Weakland T. How Behavioral Economics Can Help Cure the Health Care Crisis. Harvard Business Review. https://hbr.org/2010/03/how-behavioral-economics-can-h. Published March 1, 2010. Accessed July 16, 2019.
- Sherman E. U.S. Health Care Costs Skyrocketed to $3.65 Trillion in 2018. Fortune. https://fortune.com/2019/02/21/us-health-care-costs-2/. Published February 21, 2019. Accessed July 16, 2019.
- Abraham T. 1 in 5 patients at high risk of socioeconomic health problem, survey finds. Healthcare Dive. https://www.healthcaredive.com/news/1-in-5-patients-at-high-risk-of-socioeconomic-health-problem-survey-finds/544233/. Published December 12, 2018. Accessed July 16, 2019.
