By: Chloe Richard
 The importance of addressing mental health has grown increasingly evident as more people report negative mental health symptoms in recent years. In 2017-2018, 19% of adults experienced symptoms of a mental illness, over 1.5 million more people than the previous year.1 The most common types of mental illnesses in the United States (U.S.) are depression and anxiety. In fact:
The importance of addressing mental health has grown increasingly evident as more people report negative mental health symptoms in recent years. In 2017-2018, 19% of adults experienced symptoms of a mental illness, over 1.5 million more people than the previous year.1 The most common types of mental illnesses in the United States (U.S.) are depression and anxiety. In fact:
- About 16 million American adults experience symptoms of depression every year.2
- About 1 in every 6 adults will have depression at some point in their lives.2
- A whopping 40 million adults in the U.S. suffer from anxiety disorders every year.3
Mental Health America reports that the prevalence of mental illness was increasing even pre-COVID-19, with the pandemic further exacerbating this public health issue.1,4 As Americans have been dealing with the many stressors that have surfaced over the past year, 30.9% of people surveyed by the CDC have reported symptoms of an anxiety or depressive disorder. These stressors, such as concerns around COVID-19, the future of America, parenting through a pandemic, work and financial disruptions, and discrimination, are unlikely to disappear overnight.
If someone has an untreated, or undertreated mental illness, it can significantly impact all facets of their daily life. It can cause challenges at work or school, in relationships with others, and an overall decrease in their quality of life. It can also result in suicide, which is a leading cause of death in the U.S., claiming the lives of over 48,000 people in 2018.5
Despite the clear patient need and desire for access to mental health care, 24% of adults with a mental illness report an unmet need for treatment. This number has not decreased in the past decade.1 The inability for people to access and receive the care they need can be due to a variety of reasons, such as:
- Cost of care and insufficient insurance coverage
- Access to care, as evidenced by limited availability of treatment providers, and long wait times to be seen
- Patients’ lack of awareness of where and how to seek treatment
- Social stigma
- Transportation
- Inequity
The accessibility of community pharmacies offers an opportunity to help address some of these concerns and offer greater access to patients in need, with nearly 91% of Americans living within 5 miles of a community pharmacy.6 Furthermore, pharmacists can help identify medication problems, improve patient understanding of how to take medications, and support patient medication adherence.
Community pharmacies have been increasingly involved in public health efforts to provide screening and referrals for patients who may have depression. Screenings for other mental health conditions are also becoming more widespread. In addition, given their accessibility, pharmacies may be able to provide expanded support to this population.7 Since many people visit their pharmacy more often than their primary care physician, pharmacists can use their frequent touchpoints and existing relationships with patients to improve patient access to important screening, mental health education, and linkage to follow up care. Through enhanced patient care, community pharmacies can help to:
- Recognize symptoms and screen for mental illness
- Ensure safe and effective psychiatric medication use
- Provide patient education around mental illness and symptom management
- Provide referrals to appropriate treatment providers
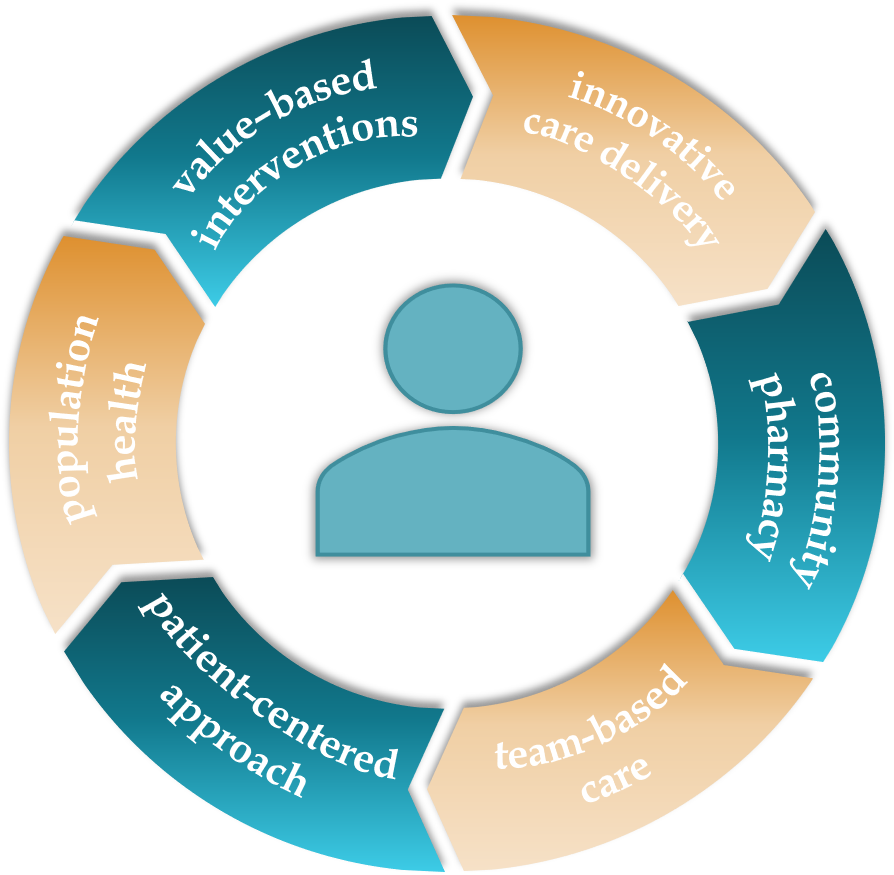
As part of the Community-based Value-driven Care Initiative (CVCI), the Center for Medication Optimization (CMO) is looking to further explore how community pharmacy can provide population health patient care interventions and help address mental health needs. A behavioral health clinical intervention for depression and anxiety support was one of four patient-centered, quality-driven interventions selected within the larger initiative to improve patient care and population health.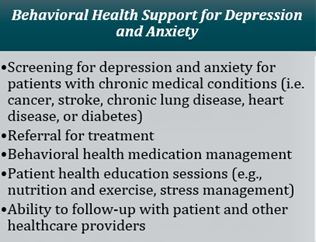 Four community pharmacy organizations will deliver this intervention by providing screenings, medication management, health education, and coordination of care over the course of one year. Through this intervention we aim to optimize behavioral health medication therapy for patients, increase patients’ understanding of depression and anxiety and related health education topics, and ultimately decrease their symptoms of depression and anxiety.
Four community pharmacy organizations will deliver this intervention by providing screenings, medication management, health education, and coordination of care over the course of one year. Through this intervention we aim to optimize behavioral health medication therapy for patients, increase patients’ understanding of depression and anxiety and related health education topics, and ultimately decrease their symptoms of depression and anxiety.
In what other ways can pharmacy help address the need for additional mental health care? Comment below to share your ideas and other thoughts on this topic.
Interested in knowing more about the project? Sign up to receive email updates on the CVCI project, blog posts, and presentations. You can also find more details about the CVCI here, and by following us on Twitter, @unc_cmo.
References:
- Mental Health America. The state of mental health in America [Internet]. [cited 2021 Apr 9]. Available from: https://mhanational.org/issues/state-mental-health-america
- Centers for Disease Control and Prevention. Mental health conditions: Depression and anxiety [Internet]. [cited 2021 Apr 9]. Available from: https://www.cdc.gov/tobacco/campaign/tips/diseases/depression-anxiety.html
- Anxiety & Depression Association of America. Facts & statistics [Internet]. [cited 2021 Apr 9]. Available from: https://adaa.org/understanding-anxiety/facts-statistics
- American Psychological Association. Stress in America 2020: A national mental health crisis [Internet]. [cited 2021 Apr 9]. Available from: https://www.apa.org/news/press/releases/stress/2020/sia-mental-health-crisis.pdf
- National Institute of Mental Health. Suicide [Internet]. [cited 2021 Apr 9]. Available from: https://www.nimh.nih.gov/health/statistics/suicide.shtml
- National Association of Chain Drug Stores. Face-to-face with community pharmacies [Internet]. [cited 2021 Apr 9]. Available from: https://www.nacds.org/pdfs/about/rximpact-leavebehind.pdf
- Kyle JA. The role of the community pharmacist in mental health. US Pharm. 2018;43(11):13–20.