By: Tazche L. Turner
Value-based care delivery models are not just limited to Accountable Care Organizations (ACO), health systems and health plans. UNC Eshelman’s School of Pharmacy Practice Advancement and Clinical Education (PACE) Division is expanding the reach of value-based care to community pharmacies through their project, Community-based Value Care Initiative (CVCI). The CVCI project is funded by the National Association of Chain Drug Stores (NACDS) Foundation. Clinical Interventions will be implemented and evaluated within community pharmacies throughout the country. The interventions are focused in the areas of Diabetes, Cardiovascular Disease, and Behavioral Health. This research project aims to improve patient care and advance population health while developing sustainable models for community pharmacy-based patient care over the long term. Specifically, project aims include:
- Identifying clinical interventions that fill current gaps in population health.
- Implementing and evaluating those interventions in the community pharmacy setting.
- Working to develop and disseminate resources to educate health care providers.
Through this article we will focus in on aim 3 and the development of sustainable models and the dissemination of project findings.
Value-based care links healthcare payments to improving quality and patient outcomes. This linkage grants patients the opportunity to receive the best care at the lowest cost to them and subsequently the healthcare system. The Institute of Medicine defines quality as “the degree to which health care services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge.”1 By providing quality care at every point of contact in the patient’s journey, we can further improve population and patient health while reducing the overall costs of healthcare. Community pharmacies are highly accessible and community pharmacists are trusted by patients, which makes them an optimal access point to support population health interventions. With the expansion of value-based interventions through these pharmacies, there is the potential to enhance access to care, address current gaps in care, and support ongoing health education for the patient. The CVCI research team is hopeful this will lead to more team-based care and better patient outcomes.
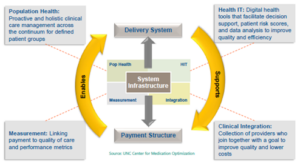
Integrating pharmacy is complex, as value-based care is a multi-faceted model dependent on quality measurement, population health, health information technology, and clinical integration of providers.2 CVCI hopes to create models to test value-based interventions in the local pharmacies that fill current population health gaps and bridge engagement between local providers and payers to promote sustainability for accessible clinical care interventions for patients. The goal is to ultimately facilitate relationships across all three groups to expand important patient care services within local communities to achieve better patient care together.
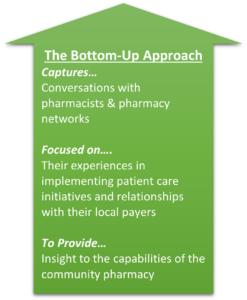
The CVCI project is utilizing a Top-Down, Bottom-Up methodology to support sustainability opportunities that can enable long standing implementation strategies.
By working Top-Down and Bottom-Up, we meet in the middle at the community level to create interventions that are sustainable by the payer and feasible by the pharmacist. Unifying them under their shared goal, to promote better care for the patients they jointly serve. Currently, the CVCI team has conducted interviews with all the pharmacy networks across all the interventions. In late June, the CVCI team reconvened the ESG to validate the population health environmental scans and provide insights into establishing payer-pharmacy collaborations at the local level. We hope to identify and produce sustainability case studies across all three interventions.
In parallel, CVCI interventions are being implemented at many local pharmacies across the country!
I’d like to thank Courtney Humphries and Jon Easter for their insights and assistance creating this blog.
Interested in learning more about the project?
Come back here to check out future blogs and follow us on Twitter @unc_pace for updates. Read more about the project here.
Tazche L. Turner is a PharmD candidate at the UNC Eshelman School of Pharmacy.
References
- Understanding Quality Measurement. Content last reviewed June 2020. Agency for Healthcare Research and Quality, Rockville, MD. https://www.ahrq.gov/patient-safety/quality-resources/tools/chtoolbx/understand/index.html
- Easter J and Pezzino N. Top-Down and Bottom-Up: Integrating Holistic Perspectives to Deliver Patient Care Interventions in Community Pharmacy. Oral presentation at: Pharmacy Quality Alliance (PQA) Annual Meeting; May, 2022; Baltimore, MD.